Platelet Rich Plasma (PRP)
What is PRP?
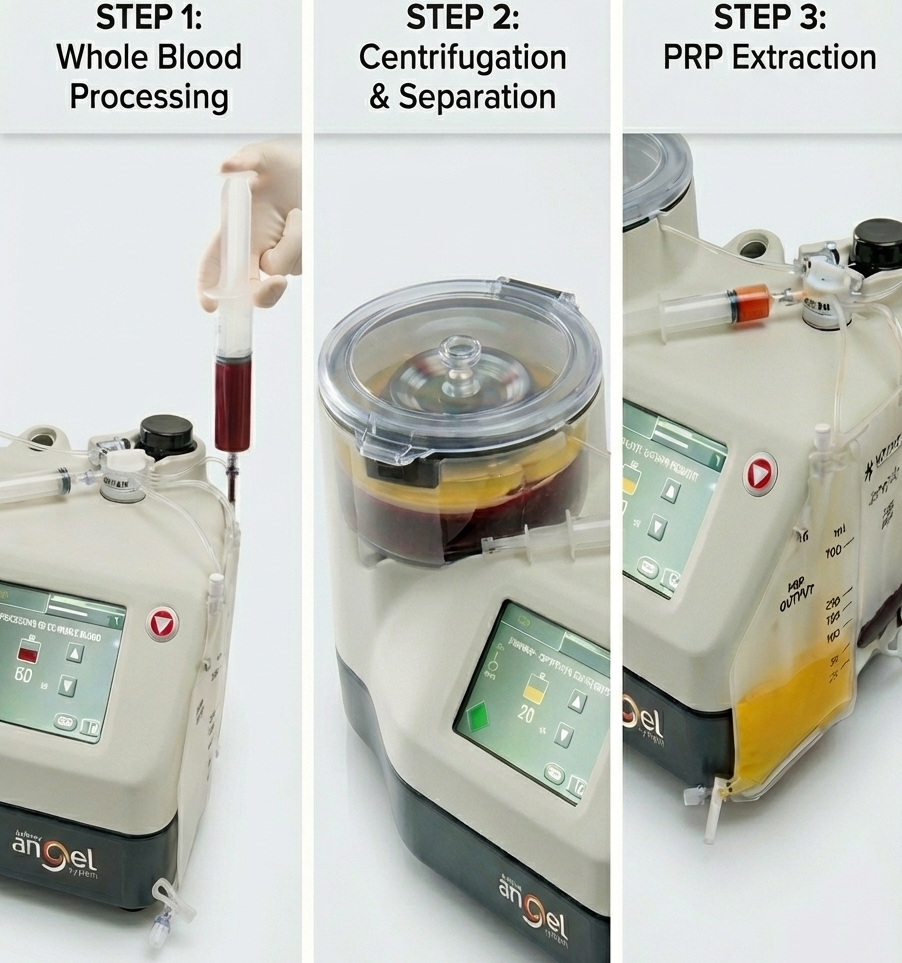
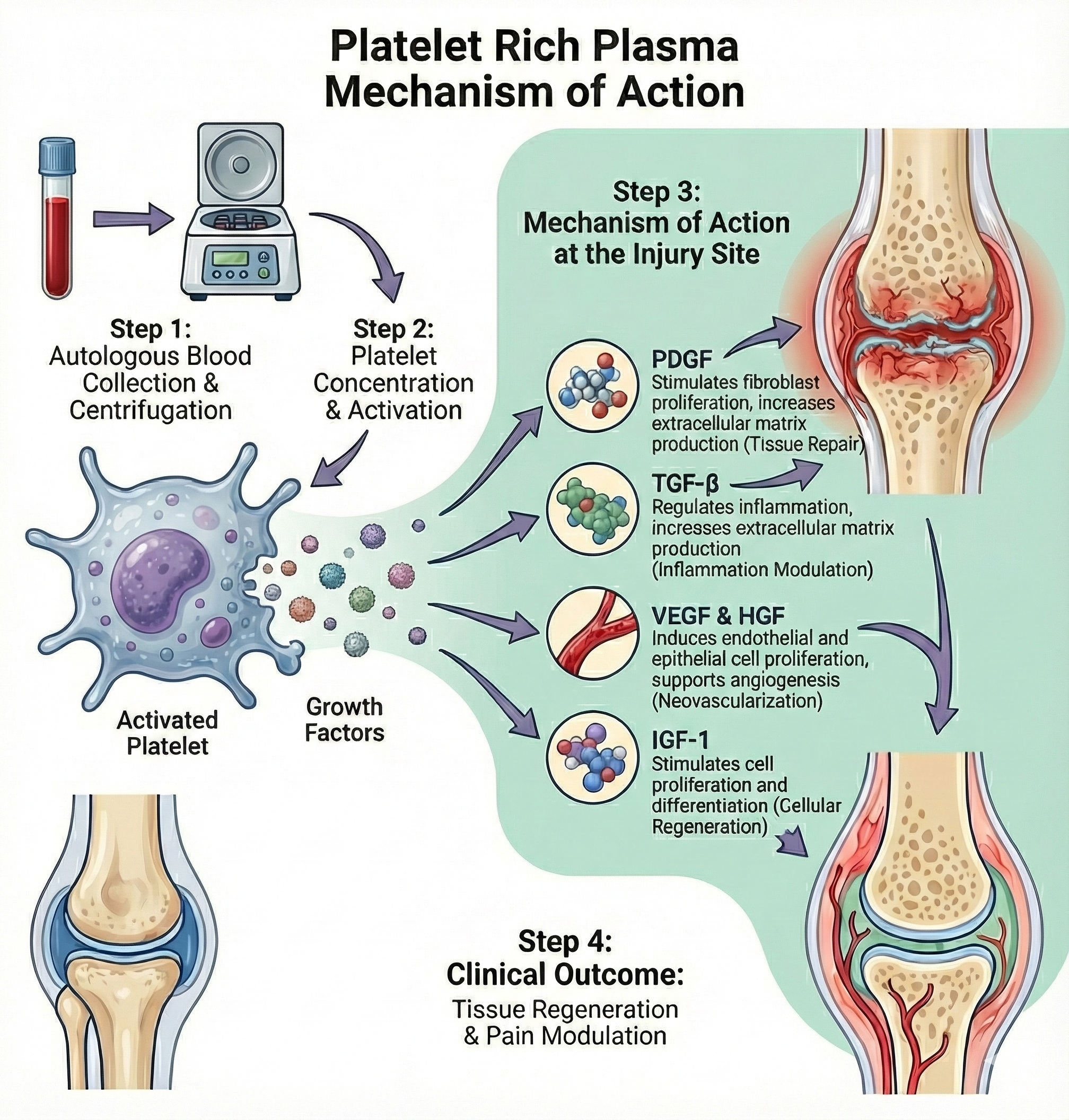
Platelet-rich plasma (PRP) is an autologous blood product with a higher than normal concentration of platelets, used in a variety of musculoskeletal applications. Its primary mechanisms are thought to involve the delivery of growth factors and cytokines that modulate inflammation and promote tissue healing and regeneration.
What is PRP used for?
The most established musculoskeletal indications for PRP are knee osteoarthritis and tendinopathies. It is primarily indicated in patients who have failed to adequately improve with conservative therapy and are not candidates for or do not want surgical intervention.
Knee Osteoarthritis
For knee osteoarthritis, multiple systematic reviews and meta-analyses, as well as consensus guidelines from the American Society of Pain and Neuroscience, support that intra-articular PRP injections provide greater pain relief and functional improvement compared to hyaluronic acid or placebo, with benefits persisting up to 12 months. PRP is generally considered safe, with adverse event rates similar to other injectates. However, optimal dosing, frequency, and formulation (leukocyte-rich vs. leukocyte-poor) remain areas of ongoing research and are not standardized in current practice.[1][3]
Tendinopathies
In tendinopathies, the American Medical Society for Sports Medicine notes the strongest evidence for PRP in lateral epicondylopathy (tennis elbow), with positive results also reported for gluteus medius tendinopathy and plantar fasciopathy.
Data for rotator cuff tendinopathy and augmentation of rotator cuff repair are promising but less definitive, while results for Achilles and patellar tendinopathies are mixed. PRP is also being explored for partial hamstring tears and as an adjunct in surgical repair of tendons and ligaments, though evidence is variable and complicated by heterogeneity in PRP preparation and study design.[4-6]
Overall, PRP is a low-risk, minimally invasive option for select musculoskeletal conditions, particularly knee osteoarthritis and certain tendinopathies, but further standardization and high-quality trials are needed to clarify its optimal use.[4][3][5-6]
References
1.Consensus Guidelines on Interventional Therapies for Knee Pain (STEP Guidelines) From the American Society of Pain and Neuroscience. Hunter CW, Deer TR, Jones MR, et al. Journal of Pain Research. 2022;15:2683-2745. doi:10.2147/JPR.S370469.
2.Platelet-Rich Plasma for Intra-Articular Injections: Preclinical and Clinical Evidence. Boffa A, Filardo G. Methods in Molecular Biology (Clifton, N.J.). 2023;2598:381-390. doi:10.1007/978-1-0716-2839-3_28.
3.Editorial Commentary: Platelet-Rich Plasma for Musculoskeletal Conditions Is Supported by a Large Number of Clinical Studies, Particularly for Knee Osteoarthritis. Hohmann E.Arthroscopy : The Journal of Arthroscopic & Related Surgery : Official Publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2024;40(2):478-480. doi:10.1016/j.arthro.2023.09.018.
4.Platelet-Rich Plasma: Fundamentals and Clinical Applications. Sheean AJ, Anz AW, Bradley JP. Arthroscopy : The Journal of Arthroscopic & Related Surgery : Official Publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2021;37(9):2732-2734. doi:10.1016/j.arthro.2021.07.003.
5.American Medical Society for Sports Medicine Position Statement: Principles for the Responsible Use of Regenerative Medicine in Sports Medicine. Finnoff JT, Awan TM, Borg-Stein J, et al.Clinical Journal of Sport Medicine : Official Journal of the Canadian Academy of Sport Medicine. 2021;31(6):530-541. doi:10.1097/JSM.0000000000000973.
6.Molecular and Biologic Effects of Platelet-Rich Plasma (PRP) in Ligament and Tendon Healing and Regeneration: A Systematic Review. Chalidis B, Givissis P, Papadopoulos P, Pitsilos C.International Journal of Molecular Sciences. 2023;24(3):2744. doi:10.3390/ijms24032744.